Spinal surgery has long been a critical area of medical care, requiring extreme precision and thorough planning to ensure positive outcomes. As technology changes, traditional spinal surgery methods are being complemented and, in some cases, replaced by robotic-assisted techniques that promise greater accuracy and improved recovery. Dr. Larry Davidson, a leader in spinal surgery, recognizes that comparing these two approaches is essential for understanding their respective benefits and limitations. With patient safety and long-term results at the forefront, both methods continue to play important roles in modern spinal care.
Traditional spinal surgeries, which have been the mainstay for decades, rely heavily on the surgeon’s expertise and manual precision. Robotic-assisted procedures, while newer, are gaining traction for their ability to enhance surgical planning and execution. Each approach brings unique advantages and challenges, making it important to assess them through a balanced lens.
Understanding Traditional Spinal Surgery
Traditional spinal surgery involves open or minimally invasive procedures in which surgeons use manual tools to correct spinal issues such as herniated discs, spinal stenosis or scoliosis. These surgeries require deep anatomical knowledge, steady hands and the ability to adapt to intraoperative changes. The technique has been refined over decades and remains a standard of care in many hospitals worldwide.
One of traditional surgery’s key strengths is its adaptability. Experienced surgeons can make real-time decisions during procedures based on direct visual and tactile feedback. In cases where complications arise unexpectedly, the ability to respond without technological mediation can be a significant advantage.
Traditional surgery is not without its challenges. Larger incisions are often required, leading to more tissue disruption, a higher risk of infection and longer recovery times. The potential for human error is also greater due to the reliance on manual instrument handling and the complexity of spinal anatomy.
Exploring Robotic-Assisted Spinal Surgery
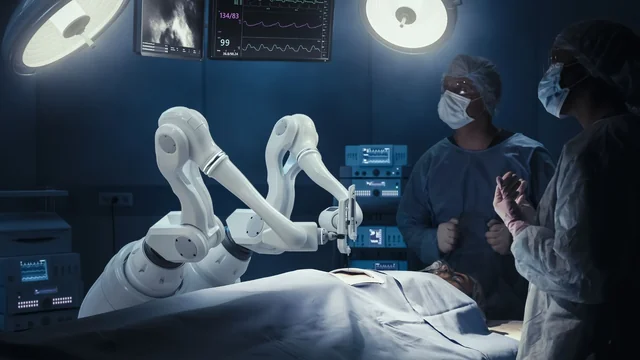
Robotic-assisted spinal surgery involves using computer-guided robotic systems to support the surgeon in executing precise movements and placements. These systems incorporate real-time imaging, 3D modeling and AI-driven planning tools to enhance accuracy. Robotic technology acts as an extension of the surgeon’s hands, offering increased stability and control.
The process often begins with preoperative planning using CT scans or MRIs. The surgeon maps out the procedure in a virtual environment, which the robotic system then translates into exact intraoperative movements. During surgery, the robot assists with guiding tools and implants, ensuring optimal placement with minimal deviation.
One of the most significant benefits of robotic-assisted surgery is the reduction in soft tissue damage. With smaller incisions and higher precision, patients often experience less blood loss, reduced postoperative pain and quicker rehabilitation. The consistent accuracy of robotic systems also helps lower the rate of revision surgeries.
Side-by-Side Comparison: Key Pros and Cons
When comparing traditional and robotic-assisted spinal surgeries, it’s important to weigh the pros and cons of each method:
Traditional Spinal Surgery Pros:
- Proven and well-established techniques
- Greater flexibility during surgery
- Accessible in a wider range of healthcare settings
- Effective for complex cases requiring direct visualization
Traditional Spinal Surgery Cons:
- Larger incisions and more invasive
- Longer recovery times
- Higher risk of infection and blood loss
- Greater dependence on surgeon experience alone
Robotic-Assisted Surgery Pros:
- Enhanced precision and accuracy
- Smaller incisions with less tissue disruption
- Faster recovery and reduced hospital stays
- Integrated with imaging and data analytics for better planning
Robotic-Assisted Surgery Cons:
- High cost and limited availability
- Requires specialized training
- Longer setup and calibration times
- Not suitable for all spinal conditions
The Role of Surgeon Expertise and Technology Integration
While robotic-assisted surgery offers technological advantages, it is ultimately the surgeon’s skill and decision-making that determine outcomes. Technology acts as a tool, not a replacement. Successful surgeries require a fusion of human expertise and robotic precision.
Dr. Larry Davidson explains, “AI will enable us to quickly review and summarize existing medical literature regarding specific types of patients with unique medical conditions and their outcomes following certain spinal surgical procedures.” This capability supports the surgeon’s judgment by providing data-driven insights that complement the clinical experience and enhance decision-making in complex cases.
Training and adaptability also influence which approach is best for a given case. Surgeons who have extensive experience with traditional methods may prefer those in specific scenarios, especially where real-time decisions are required. Conversely, those trained in robotic systems may choose them for procedures that benefit from enhanced planning and precision.
Patient-Centered Decision Making
Ultimately, the choice between traditional and robotic-assisted spinal surgery should be guided by patient-specific factors. These include the type and severity of the spinal condition, overall health status, prior surgeries and personal preferences. A collaborative discussion between the patient and surgeon ensures that the most appropriate method is selected.
Robotic-assisted surgery may be ideal for patients seeking minimally invasive options, with faster recovery. Traditional methods might be better suited for individuals requiring complex, multi-level corrections where the surgeon’s tactile feedback is critical. In either case, ensuring that patients understand the benefits and limitations of each option is key to achieving optimal outcomes.
The Future of Spinal Surgery: Hybrid Approaches and Technological Growth
Looking ahead, the distinction between traditional and robotic-assisted surgeries may continue to blur. Hybrid approaches that combine manual skills with technological support are emerging as a new standard. Surgeons may perform parts of a procedure manually while leveraging robotic systems for specific tasks like implant placement.
Advancements in artificial intelligence, augmented reality and machine learning are also expected to refine robotic systems further. As these technologies become more accessible and cost-effective, the benefits of robotic-assisted surgery may become available to a broader patient population.
Hospitals and surgical centers are investing in training and infrastructure to support these innovations, paving the way for more personalized, data-driven care. The future can likely see a more seamless integration of robotics into surgical workflows, benefiting patients through safer and more efficient procedures.
Choosing the Right Approach for Optimal Outcomes
Both traditional and robotic-assisted spinal surgeries offer valuable tools in a surgeon’s arsenal. While traditional methods provide adaptability and are time-tested, robotic-assisted techniques bring a level of precision and consistency that modern spinal care increasingly demands. The ideal approach depends on a careful evaluation of patient needs, surgeon experience and available resources.
By continuing to advance both skill sets and technology, the medical community is moving toward a future where spinal surgery is more personalized, accurate and recovery focused. Whether through tried-and-true techniques or cutting-edge robotics, the goal remains the same: to deliver the best possible outcomes for patients.